Table of Contents
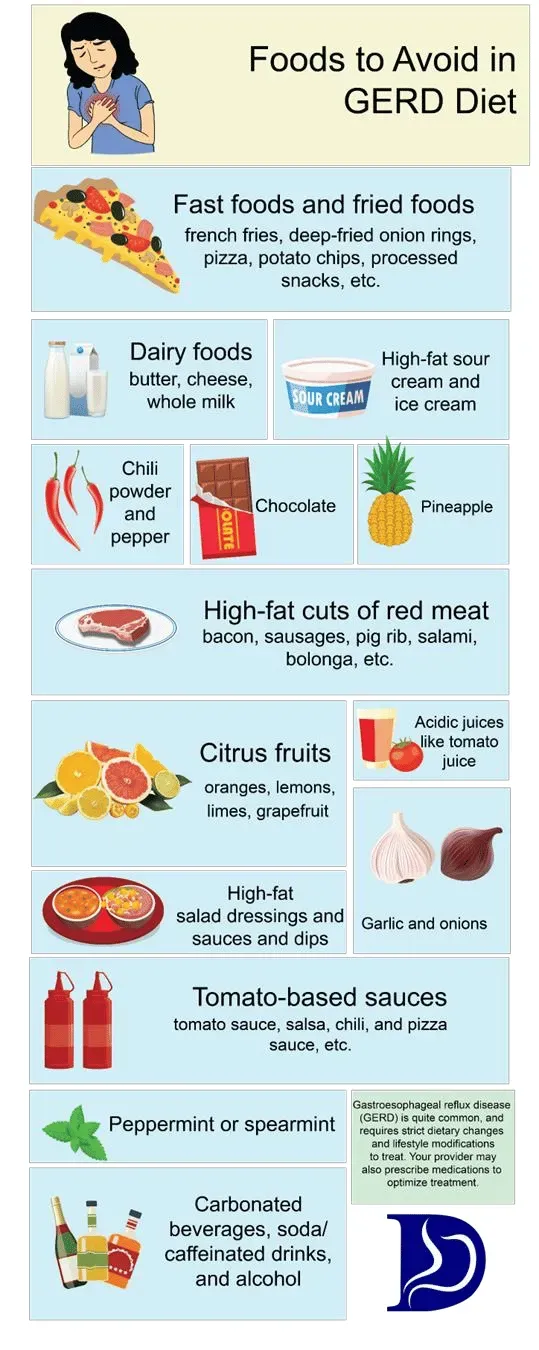
Dealing with that fiery feeling in your chest after eating? You're not alone. Acid reflux, often a symptom of GERD (Gastroesophageal Reflux Disease), is a common and frankly, annoying, problem. It happens when stomach acid splashes back up into your esophagus, causing that familiar burn known as heartburn. For many, the first line of defense isn't a pill, but a pantry raid. People start scrutinizing everything they eat and drink, desperately seeking relief.
Decoding GERD and Your Diet
Decoding GERD and Your Diet
More Than Just Heartburn: Understanding GERD
Alright, let's talk about GERD, or Gastroesophageal Reflux Disease if you want to get technical. It’s not just that occasional burn you get after inhaling a spicy pizza. We're talking about a chronic condition where stomach acid makes a regular, unwelcome trip back up your esophagus. Think of your lower esophageal sphincter (LES) as a valve. In healthy folks, it snaps shut tight after food goes down. With GERD, that valve is lazy or weak, letting acid backflow. This constant irritation can lead to inflammation, pain, and over time, potentially more serious issues. It affects a significant chunk of the population, roughly one in five people, making it a pretty big deal beyond just discomfort.
Your Plate: The First Line of Defense
When you're dealing with GERD, what you eat and drink isn't just fuel; it's battlefield strategy. Diet is often the very first thing doctors tell you to adjust, and for good reason. Certain foods and drinks can either trigger that LES to relax when it shouldn't, increase the amount of acid your stomach produces, or simply sit heavy and put pressure on that faulty valve. Ignoring your diet while trying to manage GERD is like trying to fix a leaky faucet by just mopping the floor – you're dealing with the symptom, not the source. Getting a handle on how specific foods interact with your digestive system is crucial for finding relief and improving your quality of life.
- High-fat foods (fried stuff, fatty meats, creamy sauces)
- Acidic foods (citrus fruits, tomatoes, vinegar)
- Spicy foods (anything that makes you sweat)
- Chocolate (sadly, a known LES relaxer)
- Peppermint (another LES slacker)
- Coffee and other caffeinated drinks
- Alcohol
- Carbonated beverages
Navigating the Food Minefield
So, if certain foods are the enemy, what's the game plan for your diet? It’s not about starving yourself or living on plain rice cakes forever. It’s about identifying *your* specific triggers, because everyone is a little different. While there's a list of usual suspects, your body might react badly to something unexpected, or tolerate something generally considered problematic. The core idea behind **Decoding GERD and Your Diet** involves reducing the load on your digestive system, minimizing acid production, and avoiding things that weaken that crucial LES valve. This means focusing on lower-fat options, less acidic choices, and smaller, more frequent meals rather than three huge ones.
Why Fat Matters: The Link Between Dairy and Heartburn

Why Fat Matters: The Link Between Dairy and Heartburn
The Digestive Slowdown Effect of Fat
Look, fat isn't inherently evil. Our bodies need it. But when you're battling GERD, fat throws a wrench into the digestive works in a couple of ways. First, fat takes longer to digest than carbohydrates or protein. This means food hangs around in your stomach for a longer period. A fuller stomach puts more pressure on that already compromised LES valve. Think of it like overfilling a bottle and then trying to keep the lid on tight; pressure builds, and something's going to give. More time in the stomach also means more exposure to stomach acid, which is just waiting for a chance to escape upwards.
Dairy's Double-Edged Sword: It's About the Cream
Dairy, especially the full-fat stuff, lands squarely in the "high-fat" category that gives GERD sufferers grief. That creamy texture and rich flavor? That's the fat doing its job. When that fat hits your stomach, it doesn't just slow things down; it also seems to signal that weak LES valve to relax. It’s like the valve sees the fat coming and just decides to take a break. This combination – delayed stomach emptying plus a relaxed sphincter – creates the perfect storm for acid reflux. It’s why a big glass of whole milk or a scoop of full-fat ice cream can send you scrambling for antacids faster than you can say "regurgitation."
Foods notoriously high in fat that can trigger GERD:
- Fried chicken and French fries
- Burgers and fatty cuts of steak
- Full-fat cheese and cream sauces
- Ice cream and rich desserts
- Pizza
The Fat Percentage Predicament
So, does this mean all dairy is off-limits? Not necessarily, and this is where the **low fat milk and GERD** discussion gets interesting. The issue seems tied directly to the fat content. While full-fat dairy is a common trigger due to its impact on stomach emptying and LES function, dairy with less fat might behave differently. The theory is that removing a significant portion of the fat mitigates some of these negative effects. It might not sit as heavy, and it might not be as potent a signal for that LES valve to loosen up. It's a key distinction when trying to figure out which dairy products, if any, you can tolerate.
Does Low Fat Milk Help GERD Symptoms?

Does Low Fat Milk Help GERD Symptoms?
The Buffering Myth vs. Reality
let's get right to the question on everyone's mind: can sipping on **low fat milk and GERD** symptoms coexist peacefully, maybe even beneficially? For years, the advice floated around that milk, any milk, could coat your stomach and soothe heartburn. The idea was that the liquid would wash down the acid and provide a temporary barrier. And sure, for a fleeting moment, drinking *any* liquid might feel like it's helping because it dilutes the acid. But the "coating" effect? That's largely a myth, especially with full-fat milk which, as we discussed, often makes things worse by relaxing that LES valve.
Low fat milk is a bit different. It lacks the high fat content that slows down digestion and signals the LES to loosen up. Some sources suggest that the calcium and protein in skim or low-fat milk *might* offer a slight, temporary buffering effect against stomach acid. Think of it less like a protective paint job and more like throwing a small bucket of water on a bonfire – it might damp it down for a second, but it won't put it out, and the fire might just flare back up. The relief, if any, is often short-lived.
What the Science (and Experience) Says
While the buffering idea sounds nice on paper, the real-world results for **low fat milk and GERD** are mixed. Some people report feeling a little better after drinking a small amount of low-fat milk, experiencing that brief dilution effect. Others find it does absolutely nothing, or even makes their symptoms worse. Why the discrepancy? Likely due to individual triggers and the fact that milk, even low-fat, contains lactose and protein which can stimulate acid production in some people. It's not a universal fix like, say, avoiding deep-fried everything.
Studies looking specifically at low-fat dairy and GERD symptoms haven't always delivered a definitive thumbs-up. Some research indicates no significant benefit over avoiding milk entirely, while others note the potential temporary buffering. It really boils down to personal experimentation. If you're curious, try a small amount of skim or 1% milk when you feel mild heartburn and see how *your* body reacts. Don't expect miracles, and if it makes you worse, ditch it. It's certainly not the magic bullet many hope for.
Comparing Milk Options and Potential GERD Impact:
- Whole Milk: High in fat, likely to trigger or worsen symptoms by delaying emptying and relaxing LES. Generally not recommended.
- Low-Fat Milk (1% or 2%): Lower fat, less likely to delay emptying than whole milk. May offer temporary, minor buffering for some due to calcium/protein. Individual results vary greatly.
- Skim Milk (Non-fat): Lowest fat. Similar potential for temporary buffering as low-fat milk. Still contains lactose/protein which could be an issue for some.
- Plant-Based Milks (Almond, Soy, Oat - unsweetened): Often lower in fat and acidity than dairy. Can be good alternatives, but check ingredients for added sugars or oils that might cause issues. Soy milk can be problematic for some.
Beyond Milk: Other Foods and Steps for Managing GERD

Beyond Milk: Other Foods and Steps for Managing GERD
Befriending the Right Foods
Alright, so we've poked at low fat milk and GERD, finding it's not the magic potion some hoped for. But managing this acid situation is far from hopeless. It starts with filling your plate with allies, not enemies. Think high-fiber foods that keep things moving through your digestive tract without hanging around to cause trouble. Oatmeal for breakfast? Excellent choice. Brown rice or quinoa with dinner? Thumbs up. Root vegetables like carrots and sweet potatoes are generally well-tolerated. Green beans and broccoli usually get a pass too, though some folks find broccoli causes gas, which can also pressure that LES valve. It's about building a foundation of foods that are easy on your system and don't provoke an acid uprising.
Dodging the Usual Suspects (Again)
While we touched on triggers, it bears repeating because avoiding them is half the battle. Beyond the obvious fatty and fried offenders, pay close attention to the acidic heavy hitters: tomatoes and tomato-based sauces, citrus fruits (oranges, lemons, grapefruits), and vinegar. Even seemingly healthy options like a big salad with vinaigrette can send you into a tailspin. Spicy foods are another common culprit – that burning sensation on your tongue can translate lower down, too. And yes, the heartbreak foods: chocolate, peppermint, and coffee are notorious for telling your LES valve to take a break. It feels unfair, I know, but sometimes giving these up, or at least drastically cutting back, is the key to peace.
- Foods Often Tolerated Well:
- Oatmeal
- Bananas
- Melons (cantaloupe, honeydew)
- Brown rice
- Lean meats (grilled chicken or fish)
- Green beans
- Carrots
- Ginger (often as tea)
Simple Shifts for Significant Relief
Managing GERD isn't just about *what* you eat, but *how* and *when*. Eating smaller meals more frequently, say four or five small meals instead of three big ones, prevents your stomach from getting overly full and putting pressure on the LES. Gravity is your friend here, so don't lie down right after eating – give it at least two or three hours before hitting the couch or bed. Elevating the head of your bed by about six to eight inches can also help keep acid where it belongs while you sleep. Losing even a little bit of weight if you're overweight can make a huge difference, as excess abdominal fat can squeeze your stomach and push acid upwards. These aren't glamorous fixes, but they're practical steps that often provide real relief.
Wrapping Up: Navigating GERD and Your Dairy Choices
So, where does this leave us with low fat milk and GERD? The evidence suggests that while full-fat dairy might be a trigger for some due to its fat content, low-fat or nonfat milk could potentially offer temporary relief by acting as a buffer. It's not a miracle cure, and for many, the benefits are marginal or non-existent. Diet is a significant piece of the GERD puzzle, but it's not the only piece. Focusing solely on one food item, even something as common as low fat milk, won't magically fix everything. Pay attention to your personal triggers, consider overall dietary patterns – less fat, less spice, smaller meals – and remember that sometimes, professional medical advice is the most effective strategy when lifestyle changes fall short.